Acute myeloid leukaemia (AML) is characterised by uncontrolled proliferation of myeloid progenitor cells with impaired myeloid differentiation which results in an accumulation of immature cells in the bone marrow that rapidly interfere with the generation of normal blood cells. AML is one of the most common leukaemia in adults which accounts for 25% of all adult leukaemia. The average age of AML patients is 65+ years and older patients are predisposed to higher incidence of relapse. AML consists of a variety of subtypes with different clinical characteristics and the t(8;21) AML is one of the best‐studied subtypes at the molecular level.
Although t(8;21) AML patients have a relatively favourable prognosis, this is not the case for elderly patients who are unable to tolerate intensive chemotherapy and many t(8;21) patients will relapse after initial remission. Therefore, new drugs or new personalised therapies are needed. Since drug development cannot start with patients, model systems that recapitulate aspects of specific AML sub‐types are crucial for the understanding and development of effective treatments. This review provides a comprehensive overview of the in vivo and in vitro model systems that were developed (Fig. 1) to gain insights into the global mechanisms of RUNX1‐ETO fusion, their advantages and disadvantages and what we have learned from such experiments.
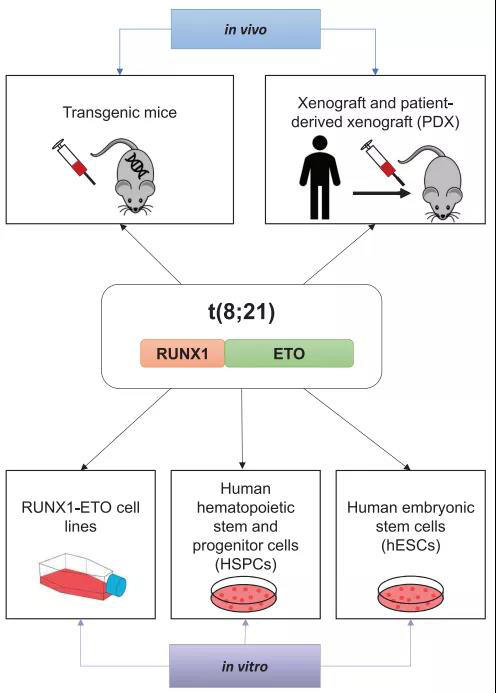
Fig.1
Article Access: https://onlinelibrary.wiley.com/doi/full/10.1002/mco2.30
Website for MedComm: https://onlinelibrary.wiley.com/journal/26882663
Looking forward to your contributions.







